Cerebrovascular Disorders
Stroke, TIA, cerebral venous sinus thrombosis and vascular malformations (AVMs, cavernomas) require fast recognition, accurate diagnosis, and coordinated care to protect brain function and independence.

Stroke (ischaemic or haemorrhagic)
Focal aware/impaired awareness: déjà vu, rising stomach sensation, unusual smells/tastes, staring, lip-smacking, one-sided jerks.
Generalised: absence (brief “blank” spells), myoclonic jerks, atonic drops, or generalised tonic–clonic seizures with loss of consciousness and convulsions.
Mimics to exclude: syncope (fainting), migraine, sleep disorders (incl. parasomnias), and functional (non-epileptic) events.

Transient Ischaemic Attack (TIA)
A TIA is a short-lived episode of neurological dysfunction from temporary loss of blood flow—often a warning that a stroke could follow. Same-day specialist assessment is recommended to confirm the cause and start prevention.
What happens next
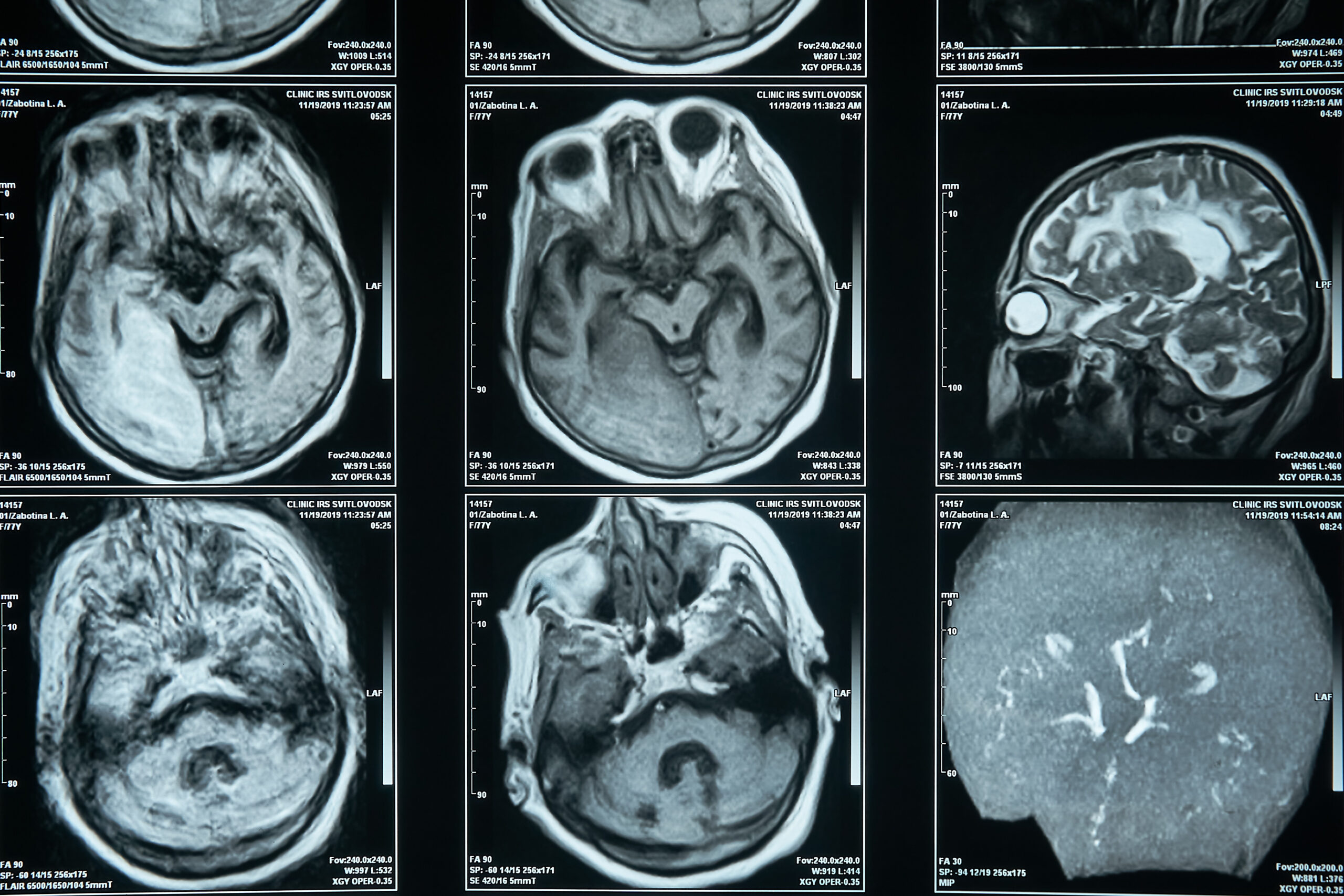
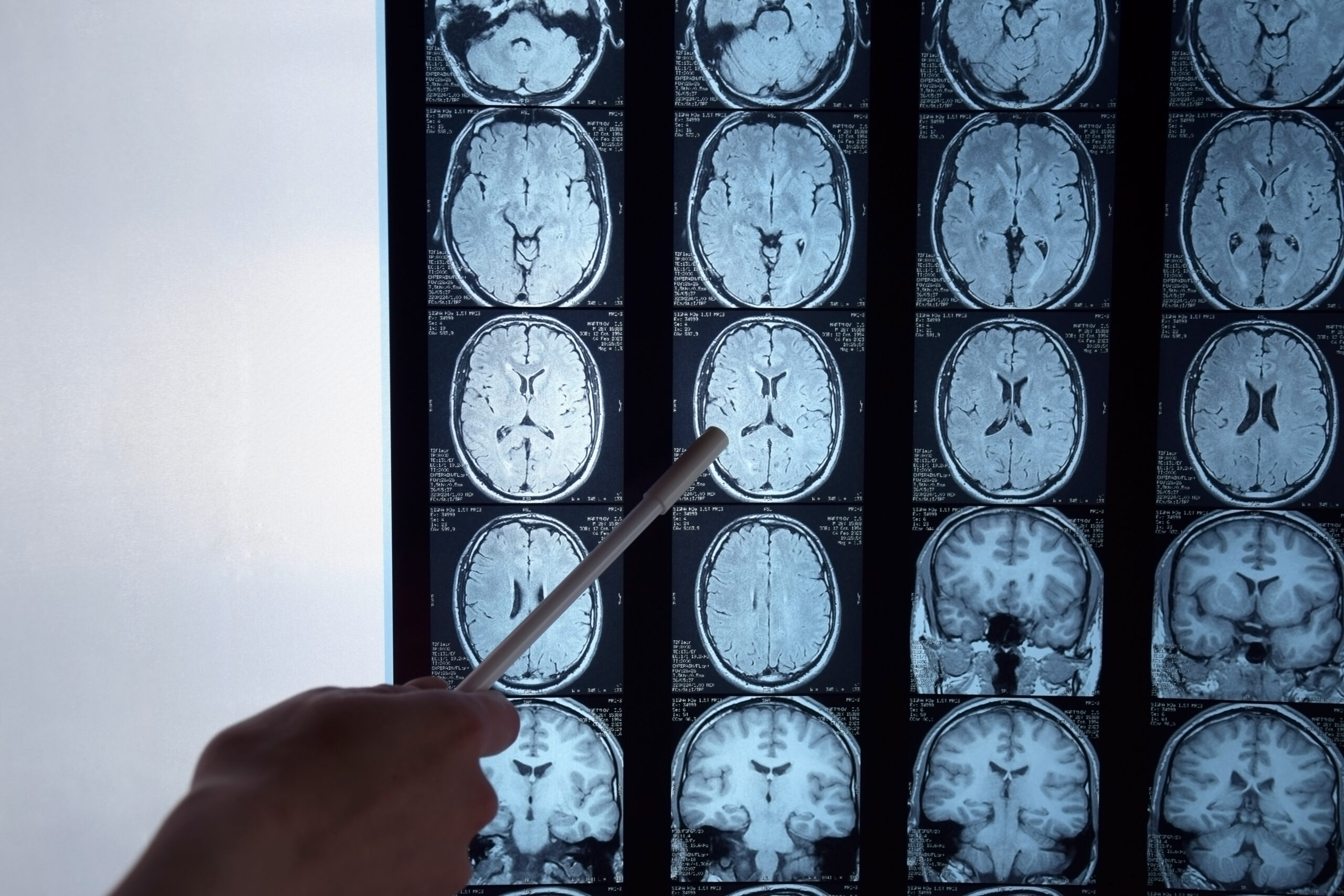
Targeted investigations (ECG/heart-rhythm monitoring, carotid/brain imaging, blood tests) and prompt treatment (for example antiplatelet therapy, blood-pressure and risk-factor management; carotid intervention in selected cases) lower early stroke risk.
Cerebral Venous Sinus Thrombosis (CVST)
CVST is a clot in the brain’s venous sinuses that can present with severe headache, seizures, focal deficits or visual symptoms. Unlike arterial stroke, first-line treatment is therapeutic anticoagulation, with seizure control and management of raised intracranial pressure as needed.
Follow-up & duration
The length of anticoagulation depends on whether a provoking factor is identified; imaging follow-up helps guide decisions. Plans are individualised.
Vascular malformations (AVMs, cavernomas)
AVMs are tangles of arteries and veins that bypass capillaries, increasing the risk of bleeding or seizures. Management ranges from monitoring to embolisation, radiosurgery or microsurgical resection, depending on size, site and risk.
Cavernomas (CCM) are clusters of slow-flow vessels that may bleed or cause seizures; options include observation, seizure management and, in selected cases, surgery.
How Dr Francesco Manfredonia can help
Rapid triage & diagnosis: history, neurological examination and tailored imaging/EEG when indicated.
Integrated prevention plans: blood pressure and lipid management, antithrombotics where appropriate, lifestyle measures and rehabilitation coordination.
Specialist pathways: swift referral to stroke units, interventional neuroradiology or neurosurgery when needed, with clear communication to you and your GP.
FAQ
What are the red-flag symptoms of stroke?
Sudden face droop, arm weakness or speech problems—use FAST and call 999 immediately. Other signs include vision loss, severe headache, dizziness or one-sided numbness/weakness.
Is a TIA a “mini-stroke”?
Yes—symptoms resolve, but it signals high short-term stroke risk. Same-day specialist assessment and prevention can be lifesaving.
What tests will I need after a TIA or stroke?
Typically brain imaging, heart-rhythm checks (for atrial fibrillation), vessel imaging and blood tests; your plan is personalised to your risks.
Can you treat CVST with blood thinners if there’s bleeding on the scan?
In specialist care, anticoagulation is usually recommended for CVST even when haemorrhage is present, with close monitoring
What’s the difference between an AVM and a cavernoma?
AVMs are fast-flow tangles connecting arteries to veins; cavernomas are slow-flow clusters of small vessels. Both can bleed or cause seizures but are managed differently.
How do you decide between surgery, radiosurgery or embolisation for an AVM?
Decisions weigh size, location, venous drainage and prior bleeding against treatment risks; complex cases are discussed in a multidisciplinary meeting.
What can I do to reduce my risk of another stroke?
Control blood pressure and lipids, take prescribed antithrombotics, stop smoking, exercise regularly and manage diabetes—tailored to your situation.
Can I fly after a stroke or TIA?
Timing depends on severity and investigations; discuss with your specialist and insurer—documentation may be required.
Will I need long-term rehabilitation?
Many people benefit from ongoing physiotherapy, occupational therapy, speech and psychological support to maximise recovery; plans are individualised.
Do seizures mean I have an AVM or cavernoma?
Not necessarily—there are many causes. If imaging shows a malformation, your team will discuss observation versus intervention based on risk.
BOOK YOUR CONSULTATION
Book a consultation with Dr Francesco Manfredonia (Dr FM) for clear diagnosis, compassionate care and a plan built around your life and goals.